J A M S E S H
Julie-Anne Minerals
Sleep Exercise Stress Hormones
Where We Put All The Pieces Of Your Puzzle Together
Knowledge is Your Super Power
Why HTMA Practitioners Say Stop Vitamin D (Even If Your Blood Test Says Low)
Vitamin D and Calcium: Two Very Different Lenses
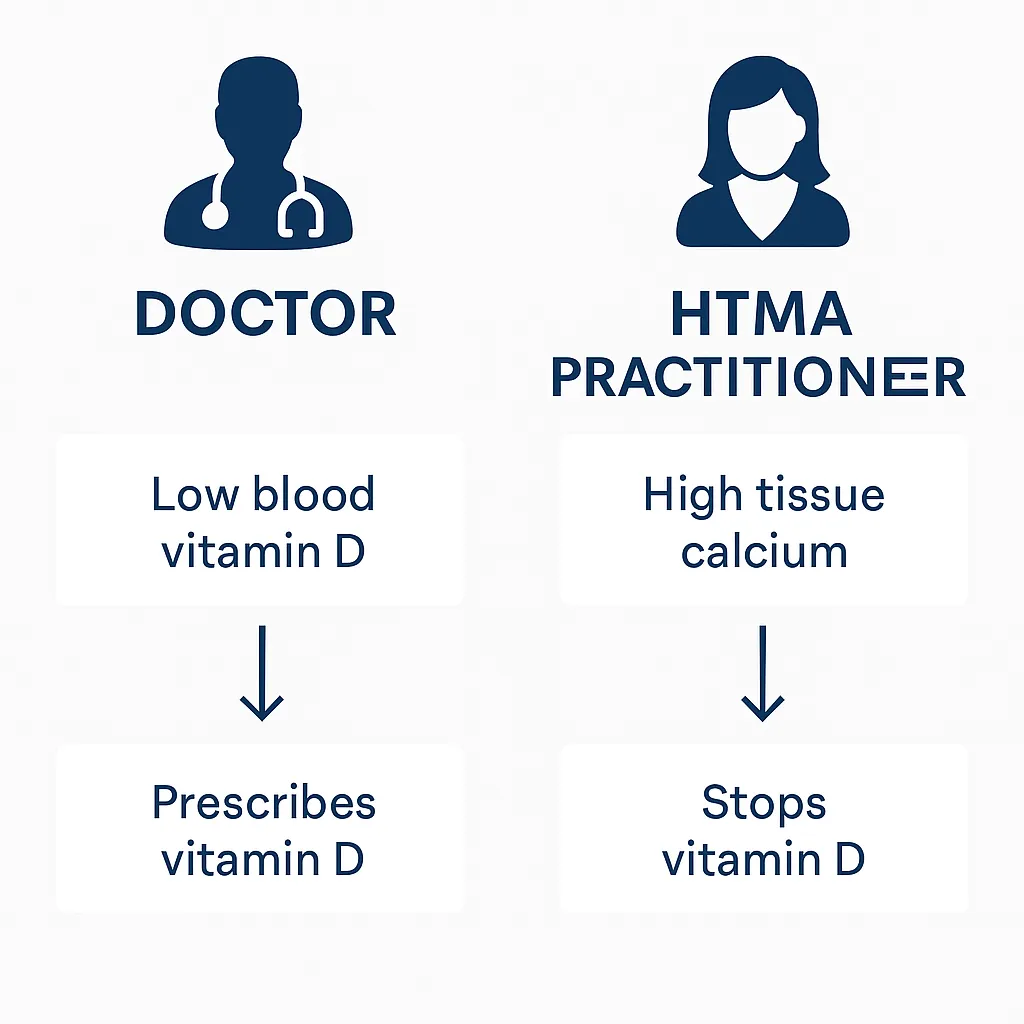
If your blood test shows low vitamin D, most doctors will recommend supplements. But if your Hair Tissue Mineral Analysis (HTMA) shows high calcium loss, an HTMA practitioner may recommend the exact opposite: stopping vitamin D altogether.
Why the difference? It comes down to whether we’re looking at a snapshot of blood or the long-term mineral regulation in tissues.
TL;DR:
Doctors see low vitamin D on bloodwork → prescribe supplements
HTMA may show high tissue calcium (or a “calcium shell”) → vitamin D makes imbalance worse
Vitamin D in this state can increase calcification, worsen adrenal burnout, and drain magnesium and potassium
HTMA practitioners often recommend stopping vitamin D until mineral regulation improves
The Blood Test Lens: Low D Means Deficiency
Bloodwork measures 25-OH vitamin D, a circulating form in the blood.
If it’s low, the assumption is: your body isn’t getting enough, so supplementing will help with bone strength, immunity, and mood.
Many doctors prescribe anywhere from 2,000 to 10,000 IU daily.
This approach works fine if the only problem is a true vitamin D deficiency.
The HTMA Lens: High Calcium = Bio-Unavailable Calcium
HTMA gives a deeper view of how your body regulates minerals over time.
When calcium is elevated, especially above 155 mg% (a “calcium shell”), it’s a sign that calcium is being:
Pulled out of bone
Deposited in soft tissues (joints, arteries, kidneys, skin)
Making you feel sluggish, stiff, and emotionally flat
This isn’t “healthy calcium.” It’s bio-unavailable calcium and the body can’t use it properly.
“If you’ve been told to take vitamin D but still struggle with fatigue, stiffness, or brain fog, your mineral system may be telling a different story. Book a consultation and we’ll get to the root cause.” Learn more about your Hair Tissue Mineral Analysis Test and Book It Today
What Happens if You Add Vitamin D Here?
Vitamin D increases calcium absorption from your gut. In a calcium loss pattern:
More calcium piles up in soft tissue instead of bone
Magnesium is drained faster. Vitamin D isn’t active right out of the capsule or from the sun. It has to be converted in the liver and kidneys into its active form (calcitriol). Each conversion step uses magnesium-dependent enzymes.
Potassium drops, worsening fatigue and thyroid sluggishness
Adrenal burnout deepens, locking in the slow oxidizer pattern
Even if you add vitamin K2, you’re still forcing calcium into a system that can’t regulate it.
Why Doctors vs. HTMA Practitioners See It Differently
Functional/medical doctor: looks at blood → sees “low vitamin D” → prescribes supplement
HTMA practitioner: looks at tissue → sees “high calcium loss” → avoids vitamin D to prevent calcification and burnout
Both are using real data. They’re just asking different questions.
So What’s the Right Approach?
If your HTMA shows high calcium, the goal isn’t more vitamin D. The goal is restoring regulation so your body can actually use the calcium it already has.
This means:
Rebuilding sodium/potassium balance to strengthen adrenal and thyroid function
Supporting magnesium to calm calcium excess
Ensuring adequate protein and phosphorus so calcium anchors into bone
Balancing copper metabolism (low ceruloplasmin often drives calcium issues)
Using natural sunlight instead of high-dose supplements
The Bottom Line
Low vitamin D on a blood test doesn’t always mean you should supplement. If your HTMA shows a calcium shell or high calcium loss, vitamin D can do more harm than good.
Blood = snapshot. HTMA = regulation.
That’s why your doctor may prescribe vitamin D, while your HTMA practitioner recommends stopping it.
“Curious about what your body is asking you for mineral wise? Learn more about HTMA testing here
© Copyright JAMSesh Fitness and Health 2026
